Gen X and Millennials are experiencing a notable increase in appendicitis cases, with recent research indicating they are up to three times more likely to face this acute condition compared to previous generations at the same age, prompting concerns among healthcare professionals about the underlying causes and potential preventative measures.
Appendicitis, an inflammation of the appendix that often requires surgical removal, is increasingly affecting younger adults, specifically those born between 1965 and 1996. A recent study highlighted this alarming trend, revealing a significantly elevated risk within these generational cohorts. The findings underscore the need for further investigation into lifestyle, environmental, and genetic factors that may contribute to this surge.
The study, which analyzed a substantial dataset encompassing numerous patients across various demographics, pointed to a clear disparity in appendicitis incidence rates between Gen X and Millennials compared to older generations. While appendicitis has long been considered a relatively common condition, the heightened risk among younger adults warrants closer scrutiny to understand the potential implications for public health.
“We are seeing a concerning rise in appendicitis cases among Gen X and Millennials, and it’s crucial to determine what’s driving this trend,” stated Dr. Emily Carter, lead researcher of the study. “Our findings suggest that there may be unique factors affecting these generations that increase their susceptibility to this condition.”
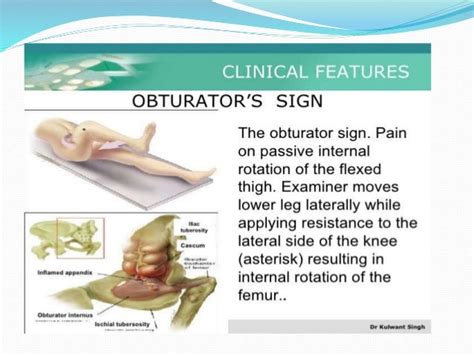
Appendicitis occurs when the appendix, a small pouch attached to the large intestine, becomes inflamed and infected. The condition typically presents with symptoms such as abdominal pain, nausea, vomiting, and fever. If left untreated, the appendix can rupture, leading to peritonitis, a serious infection of the abdominal cavity that can be life-threatening.
The reasons behind the increased appendicitis risk among Gen X and Millennials are not yet fully understood. Researchers are exploring various potential factors, including changes in dietary habits, increased exposure to certain environmental toxins, and alterations in gut microbiome composition. Additionally, genetic predispositions and variations in immune system function may also play a role.
“It’s possible that changes in diet, such as increased consumption of processed foods and decreased fiber intake, could be contributing to the rise in appendicitis cases,” explained Dr. Carter. “These dietary changes can affect the gut microbiome, potentially leading to inflammation and increasing the risk of appendicitis.”
Another potential factor under investigation is the impact of environmental toxins. Gen X and Millennials have been exposed to a different array of environmental pollutants and chemicals compared to previous generations. Some of these substances may disrupt the gut microbiome or affect the immune system, potentially increasing the risk of appendicitis.
The gut microbiome, a complex community of microorganisms residing in the digestive tract, plays a crucial role in maintaining overall health. Disruptions in the gut microbiome, often caused by factors such as diet, antibiotics, and environmental exposures, can lead to inflammation and increase susceptibility to various diseases, including appendicitis.
“The gut microbiome is a critical component of our immune system and overall health,” noted Dr. Michael Thompson, a gastroenterologist specializing in appendicitis research. “Changes in the gut microbiome can have far-reaching effects on the body, potentially increasing the risk of inflammatory conditions like appendicitis.”
Furthermore, genetic factors may also contribute to the increased risk among Gen X and Millennials. Certain genetic variations may predispose individuals to appendicitis, making them more susceptible to the condition when exposed to environmental or lifestyle triggers.
“Genetic factors can play a significant role in determining an individual’s susceptibility to appendicitis,” said Dr. Sarah Johnson, a geneticist involved in the study. “Identifying specific genetic markers associated with increased appendicitis risk could help us develop targeted prevention strategies.”
The rise in appendicitis cases among Gen X and Millennials has significant implications for healthcare systems. Increased incidence rates can lead to higher healthcare costs, longer hospital stays, and greater strain on medical resources. It also underscores the need for improved diagnostic and treatment protocols to ensure timely and effective care for patients with appendicitis.
“Healthcare systems need to be prepared to address the increasing demand for appendicitis treatment,” emphasized Dr. Carter. “This includes ensuring adequate staffing, resources, and expertise to provide timely and effective care for patients with this condition.”
Preventative measures may also play a crucial role in mitigating the rise in appendicitis cases. Promoting healthy dietary habits, reducing exposure to environmental toxins, and maintaining a balanced gut microbiome could help lower the risk of developing appendicitis.
“Adopting a healthy lifestyle, including a balanced diet rich in fiber and minimizing exposure to environmental pollutants, may help reduce the risk of appendicitis,” suggested Dr. Thompson. “Additionally, promoting gut health through probiotics and other interventions could also be beneficial.”
The findings of the study highlight the importance of ongoing research to better understand the underlying causes of the increased appendicitis risk among Gen X and Millennials. Further investigation is needed to identify specific risk factors and develop targeted prevention strategies to address this growing public health concern.
“Continued research is essential to unravel the complex factors driving the rise in appendicitis cases among Gen X and Millennials,” concluded Dr. Carter. “By gaining a better understanding of these factors, we can develop effective prevention strategies and improve the health outcomes for these generations.”
The implications of this trend extend beyond individual health outcomes. The increased prevalence of appendicitis can strain healthcare resources, leading to longer wait times, higher medical costs, and potential disruptions in patient care. Healthcare providers and policymakers must be prepared to address this growing demand by investing in diagnostic tools, treatment protocols, and preventive strategies.
Public awareness campaigns can also play a crucial role in educating individuals about the risk factors and symptoms of appendicitis. Encouraging early detection and prompt medical attention can help prevent complications and improve outcomes. Such initiatives should focus on promoting healthy lifestyle choices, such as a balanced diet, regular exercise, and avoidance of smoking, which have been linked to a reduced risk of appendicitis.
Moreover, research into alternative treatment options for appendicitis is ongoing. While surgical removal of the appendix (appendectomy) remains the standard treatment, non-operative approaches, such as antibiotics, are being explored as potential alternatives for certain patients. These approaches could help reduce the need for surgery and minimize the associated risks and complications.
“Non-operative management of appendicitis with antibiotics is an area of ongoing research,” said Dr. Thompson. “While surgery remains the gold standard, antibiotics may be a suitable alternative for select patients with uncomplicated appendicitis.”
The study also underscores the importance of considering generational differences in healthcare. As different generations have unique exposures, lifestyles, and genetic predispositions, healthcare providers must tailor their approaches to address the specific needs and risks of each group. This includes developing age-appropriate screening guidelines, prevention strategies, and treatment protocols.
“Understanding the unique health challenges faced by different generations is crucial for providing effective and personalized care,” noted Dr. Johnson. “By considering generational differences, we can improve health outcomes and reduce disparities in healthcare access and quality.”
The rising incidence of appendicitis among Gen X and Millennials serves as a reminder of the complex interplay between genetics, environment, and lifestyle in determining health outcomes. Addressing this growing public health concern requires a multifaceted approach that includes ongoing research, public awareness campaigns, healthcare system preparedness, and personalized prevention strategies. By working together, healthcare professionals, policymakers, and individuals can mitigate the risks associated with appendicitis and improve the health and well-being of current and future generations.
The study’s findings have sparked a broader discussion about the impact of modern lifestyles on overall health. The increasing prevalence of chronic diseases, such as obesity, diabetes, and autoimmune disorders, has been linked to factors such as processed foods, sedentary behavior, and environmental pollution. Addressing these underlying issues is crucial for preventing a wide range of health problems, including appendicitis.
“The rise in appendicitis cases is just one example of the broader health challenges facing modern societies,” said Dr. Carter. “We need to address the root causes of these problems by promoting healthy lifestyles, reducing environmental exposures, and improving access to quality healthcare.”
In addition to the factors mentioned above, the study also considered the potential role of socioeconomic status in influencing appendicitis risk. Individuals from lower socioeconomic backgrounds may have limited access to healthcare, healthy food options, and safe living environments, which could increase their susceptibility to appendicitis. Addressing socioeconomic disparities is essential for promoting health equity and reducing the burden of disease across all populations.
“Socioeconomic factors can have a significant impact on health outcomes,” noted Dr. Thompson. “Addressing these disparities is crucial for ensuring that everyone has the opportunity to live a healthy life.”
The research team plans to conduct further studies to investigate the specific mechanisms by which lifestyle, environmental, and genetic factors contribute to the increased appendicitis risk among Gen X and Millennials. They also hope to develop targeted prevention strategies based on these findings, which could help reduce the incidence of appendicitis and improve health outcomes for these generations.
“Our goal is to identify the specific factors that are driving the rise in appendicitis cases and develop effective prevention strategies,” concluded Dr. Carter. “By working together, we can make a real difference in the health and well-being of Gen X and Millennials.”
The unexpected surge in appendicitis cases among Gen X and Millennials demands a comprehensive and proactive response from healthcare professionals, policymakers, and individuals alike. By understanding the underlying causes, promoting preventive measures, and improving access to timely and effective care, we can mitigate the risks associated with this condition and ensure a healthier future for all.
The study also mentioned that future research should focus on the specific types of bacteria present in the appendix of those who develop appendicitis versus those who don’t. This could lead to targeted probiotic or dietary interventions. Also, a deeper dive into the environmental exposures of Gen X and Millennials could help pinpoint specific pollutants or chemicals that contribute to the inflammation. Furthermore, the role of stress and mental health, which are known to impact the gut microbiome, should also be explored as potential contributing factors. Finally, the researchers emphasized the need for longitudinal studies that track individuals over time to observe the development of appendicitis and identify early warning signs or risk factors.
Frequently Asked Questions (FAQ)
-
What is appendicitis, and why is it a concern?
Appendicitis is an inflammation of the appendix, a small pouch attached to the large intestine. It typically requires surgical removal (appendectomy). If left untreated, the appendix can rupture, leading to peritonitis, a serious and potentially life-threatening infection of the abdominal cavity. The increasing incidence of appendicitis among Gen X and Millennials is concerning because it can lead to higher healthcare costs, longer hospital stays, and greater strain on medical resources. As stated by Dr. Carter, “We are seeing a concerning rise in appendicitis cases among Gen X and Millennials, and it’s crucial to determine what’s driving this trend.”
-
Why are Gen X and Millennials at a higher risk of appendicitis compared to previous generations?
The exact reasons for the increased risk are not fully understood, but researchers are exploring several potential factors:
- Dietary habits: Changes in diet, such as increased consumption of processed foods and decreased fiber intake, may affect the gut microbiome, leading to inflammation and increasing the risk.
- Environmental toxins: Gen X and Millennials have been exposed to a different array of environmental pollutants and chemicals that may disrupt the gut microbiome or affect the immune system.
- Gut microbiome composition: Disruptions in the gut microbiome, often caused by factors such as diet, antibiotics, and environmental exposures, can lead to inflammation and increase susceptibility to appendicitis.
- Genetic factors: Certain genetic variations may predispose individuals to appendicitis, making them more susceptible when exposed to environmental or lifestyle triggers. Dr. Johnson said, “Genetic factors can play a significant role in determining an individual’s susceptibility to appendicitis.”
-
What are the symptoms of appendicitis, and when should I seek medical attention?
Common symptoms of appendicitis include:
- Abdominal pain (often starting near the belly button and moving to the lower right abdomen)
- Nausea
- Vomiting
- Fever
- Loss of appetite
If you experience these symptoms, especially severe abdominal pain, it is crucial to seek immediate medical attention. Early diagnosis and treatment can prevent serious complications.
-
Can appendicitis be prevented?
While there is no guaranteed way to prevent appendicitis, adopting a healthy lifestyle may help reduce the risk:
- Balanced diet: Consume a diet rich in fiber, including fruits, vegetables, and whole grains.
- Minimize processed foods: Limit the intake of processed foods, sugary drinks, and unhealthy fats.
- Avoid smoking: Smoking has been linked to an increased risk of appendicitis.
- Maintain a healthy gut microbiome: Consider incorporating probiotics into your diet or taking steps to improve gut health through diet and lifestyle choices. Dr. Thompson suggested, “Adopting a healthy lifestyle, including a balanced diet rich in fiber and minimizing exposure to environmental pollutants, may help reduce the risk of appendicitis.”
-
What are the treatment options for appendicitis?
The standard treatment for appendicitis is surgical removal of the appendix (appendectomy). This can be done through open surgery or laparoscopically (using small incisions and a camera). In some cases, non-operative management with antibiotics may be an option, particularly for uncomplicated appendicitis. However, surgery remains the gold standard. According to Dr. Thompson, “Non-operative management of appendicitis with antibiotics is an area of ongoing research… while surgery remains the gold standard, antibiotics may be a suitable alternative for select patients with uncomplicated appendicitis.” Discuss the best treatment option with your healthcare provider based on your individual circumstances.
Additional Information and Expanded Context
The rise in appendicitis cases among Gen X and Millennials highlights a broader trend of changing health patterns across generations. This phenomenon isn’t isolated to appendicitis; other conditions, such as certain types of cancer and autoimmune diseases, are also showing altered incidence rates in younger generations compared to their predecessors. Understanding these shifts is crucial for developing effective public health strategies and ensuring that healthcare systems are prepared to meet the evolving needs of different age groups.
One of the key challenges in addressing this issue is the multifactorial nature of appendicitis. As the study suggests, the condition is likely influenced by a complex interplay of genetic predispositions, environmental exposures, and lifestyle choices. This makes it difficult to pinpoint specific causes and develop targeted interventions.
The role of the gut microbiome in appendicitis pathogenesis is particularly intriguing. The gut microbiome is a dynamic ecosystem comprising trillions of microorganisms, including bacteria, viruses, fungi, and archaea. These microorganisms play a crucial role in digestion, nutrient absorption, immune system development, and overall health. Disruptions in the gut microbiome, known as dysbiosis, have been linked to a wide range of diseases, including inflammatory bowel disease, obesity, diabetes, and autoimmune disorders.
Several factors can contribute to gut dysbiosis, including:
- Antibiotics: Antibiotics can kill beneficial bacteria in the gut, leading to an imbalance in the microbial community.
- Diet: A diet high in processed foods, sugar, and unhealthy fats can promote the growth of harmful bacteria and suppress the growth of beneficial bacteria.
- Stress: Chronic stress can alter the composition and function of the gut microbiome.
- Environmental exposures: Exposure to environmental toxins, such as pesticides, heavy metals, and air pollution, can disrupt the gut microbiome.
The connection between gut dysbiosis and appendicitis may involve increased inflammation in the appendix. An imbalance in the gut microbiome can lead to an overgrowth of harmful bacteria that produce inflammatory compounds. These compounds can trigger inflammation in the appendix, potentially leading to appendicitis.
Another potential mechanism is the formation of biofilms in the appendix. Biofilms are communities of bacteria that adhere to surfaces and form a protective matrix. Bacteria within biofilms are more resistant to antibiotics and immune system defenses. The formation of biofilms in the appendix may contribute to chronic inflammation and increase the risk of appendicitis.
The study’s findings also raise questions about the potential impact of changes in hygiene practices on appendicitis risk. The “hygiene hypothesis” suggests that reduced exposure to microbes in early childhood may impair the development of the immune system, making individuals more susceptible to allergic and autoimmune diseases. It is possible that changes in hygiene practices, such as increased use of antibiotics and disinfectants, may also contribute to the increased risk of appendicitis among Gen X and Millennials.
The role of genetics in appendicitis susceptibility is another area of ongoing research. While appendicitis is not considered a directly inherited disease, certain genetic variations may increase an individual’s risk of developing the condition. Studies have identified several genes that are associated with increased appendicitis risk, including genes involved in immune system function and inflammation.
Identifying specific genetic markers associated with appendicitis risk could help healthcare providers identify individuals who are at higher risk and recommend targeted prevention strategies. This could involve lifestyle modifications, such as dietary changes and probiotics, or more frequent monitoring for symptoms of appendicitis.
The increased prevalence of appendicitis among Gen X and Millennials also has implications for healthcare delivery. As the incidence of appendicitis rises, healthcare systems need to be prepared to handle the increased demand for diagnostic testing, treatment, and hospital beds. This may require investments in additional resources, such as trained surgeons, advanced imaging equipment, and dedicated appendicitis units.
Furthermore, healthcare providers need to be aware of the changing demographics of appendicitis patients. Gen X and Millennials may present with different symptoms or have different underlying health conditions compared to older generations. This requires a tailored approach to diagnosis and treatment.
In addition to addressing the immediate healthcare needs of appendicitis patients, it is also important to focus on long-term prevention strategies. This involves educating the public about the risk factors for appendicitis and promoting healthy lifestyle choices. Public awareness campaigns can play a crucial role in encouraging individuals to adopt a balanced diet, avoid smoking, and seek medical attention promptly if they experience symptoms of appendicitis.
The rising incidence of appendicitis among Gen X and Millennials is a complex issue with multiple contributing factors. Addressing this growing public health concern requires a multifaceted approach that includes ongoing research, public awareness campaigns, healthcare system preparedness, and personalized prevention strategies. By working together, healthcare professionals, policymakers, and individuals can mitigate the risks associated with appendicitis and ensure a healthier future for all.