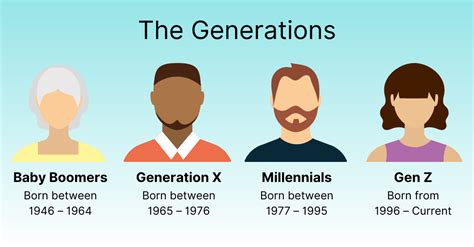
Gen X and Millennials are experiencing appendicitis at rates significantly higher—up to three times greater—than their parents’ generation, according to a recent study presented at Digestive Disease Week 2024. This alarming trend highlights a potential shift in the epidemiology of appendicitis, a common and often urgent medical condition requiring surgical intervention.
The study, which analyzed data from a large national health insurance database, revealed a noticeable increase in appendicitis cases among individuals born between 1965 and 1995 compared to those born earlier. Researchers suggest that environmental factors, changes in diet, and alterations in gut microbiome composition could be contributing to this rise. While the exact cause remains unclear, this research underscores the importance of further investigation to understand the underlying mechanisms driving this generational disparity.
Appendicitis, characterized by inflammation of the appendix, typically presents with abdominal pain, nausea, vomiting, and fever. If left untreated, it can lead to serious complications, including rupture of the appendix, peritonitis (inflammation of the abdominal lining), and sepsis (a life-threatening response to infection).
“We observed a significant increase in appendicitis diagnoses among Gen X and Millennials compared to their parents’ generation,” stated Dr. Giana Croesi, lead author of the study and a researcher at the Mayo Clinic. “This suggests that there may be generational risk factors at play that are contributing to this rise.”
The research team emphasized the need for increased awareness among healthcare providers regarding this trend to ensure timely diagnosis and treatment of appendicitis in younger adults. They also called for further research to identify the specific factors driving this generational difference, which could lead to targeted prevention strategies.
Study Details and Methodology
The study utilized data from a large national health insurance claims database, encompassing millions of patients across the United States. Researchers analyzed appendicitis incidence rates across different birth cohorts, comparing the rates among Gen X and Millennials to those of their parents’ generation (Baby Boomers and the Silent Generation).
The researchers meticulously controlled for potential confounding factors such as age, sex, race, socioeconomic status, and pre-existing medical conditions to isolate the generational effect on appendicitis risk. They calculated age-adjusted incidence rates to account for differences in age distribution across the different birth cohorts.
The analysis revealed a clear upward trend in appendicitis incidence among younger generations. The study found that Gen X and Millennials had a significantly higher risk of developing appendicitis compared to their parents, with some estimates suggesting a threefold increase.
Possible Explanations for the Increase
While the study did not pinpoint the exact cause of the increased appendicitis rates in Gen X and Millennials, the researchers proposed several potential explanations:
-
Changes in Diet: Modern diets, often characterized by processed foods, low fiber intake, and high sugar consumption, could be contributing to alterations in the gut microbiome and increased inflammation in the digestive tract. The decreased consumption of fruits and vegetables, coupled with the increased intake of refined carbohydrates, may promote an environment conducive to appendicitis development.
-
Gut Microbiome Alterations: The gut microbiome, a complex community of microorganisms residing in the digestive tract, plays a crucial role in maintaining gut health and immune function. Changes in diet, antibiotic use, and other environmental factors can disrupt the balance of the gut microbiome, leading to inflammation and increased susceptibility to appendicitis. Research suggests that certain bacterial species may be associated with an increased risk of appendicitis, while others may offer protection.
-
Environmental Factors: Exposure to environmental toxins, pollutants, and other stressors may also contribute to the rise in appendicitis cases. The increased prevalence of environmental chemicals in food, water, and air could be impacting the immune system and increasing inflammation in the appendix.
-
Increased Hygiene Hypothesis: The “hygiene hypothesis” suggests that reduced exposure to infections and pathogens in early childhood may lead to an altered immune system development, making individuals more susceptible to autoimmune diseases and inflammatory conditions, including appendicitis. The widespread use of antibiotics and improved sanitation practices may have inadvertently weakened the immune system’s ability to regulate inflammation in the gut.
-
Delayed Childbearing: Women in Gen X and Millennial generations are having children later in life as compared to their parent’s generation. Some studies indicate that delay in childbearing and reduced parity might be associated with increased risk of appendicitis.
Implications for Healthcare
The findings of this study have significant implications for healthcare providers. The increased incidence of appendicitis in Gen X and Millennials underscores the need for increased awareness and vigilance in diagnosing and treating this condition in younger adults.
Healthcare providers should be aware of the potential for appendicitis in patients presenting with abdominal pain, nausea, vomiting, and fever, regardless of age. Timely diagnosis and treatment are crucial to prevent serious complications, such as rupture and peritonitis.
The study also highlights the importance of promoting healthy lifestyle choices, including a balanced diet, regular exercise, and stress management, to potentially reduce the risk of appendicitis.
Future Research Directions
The researchers emphasized the need for further research to identify the specific factors driving the generational difference in appendicitis risk. Future studies should focus on:
-
Investigating the Role of Diet and Gut Microbiome: Conducting detailed dietary assessments and analyzing the gut microbiome composition of individuals with and without appendicitis can help identify specific dietary factors and microbial imbalances associated with increased risk.
-
Examining Environmental Exposures: Assessing exposure to environmental toxins, pollutants, and other stressors can shed light on the potential role of environmental factors in the development of appendicitis.
-
Exploring Genetic Predisposition: Investigating the genetic factors that may predispose individuals to appendicitis can help identify those at higher risk and develop targeted prevention strategies.
-
Analyzing Healthcare Utilization Patterns: Examining healthcare utilization patterns, such as antibiotic use and access to medical care, can help identify factors that may contribute to delayed diagnosis and treatment of appendicitis.
Appendicitis: A Closer Look
Appendicitis is a common condition that occurs when the appendix, a small, finger-shaped pouch extending from the colon, becomes inflamed and infected. The appendix has no known essential function in humans, and its inflammation can lead to serious complications if left untreated.
Symptoms of Appendicitis:
The classic symptoms of appendicitis include:
- Abdominal Pain: Typically starts as a dull ache around the navel and then moves to the lower right abdomen. The pain may worsen with movement, coughing, or sneezing.
- Nausea and Vomiting: Often accompany abdominal pain.
- Loss of Appetite: A common symptom of appendicitis.
- Fever: Usually low-grade, but may become higher as the infection progresses.
- Constipation or Diarrhea: Some individuals may experience changes in bowel habits.
- Abdominal Tenderness: The lower right abdomen is often tender to the touch.
Not everyone with appendicitis experiences all of these symptoms, and the symptoms may vary depending on the individual’s age, the location of the appendix, and other factors.
Diagnosis of Appendicitis:
The diagnosis of appendicitis typically involves a physical examination, a review of the patient’s medical history, and diagnostic tests.
- Physical Examination: The doctor will examine the abdomen for tenderness, guarding (muscle tightening in response to pain), and rebound tenderness (pain that worsens when pressure is released).
- Blood Tests: A complete blood count (CBC) can help detect signs of infection, such as an elevated white blood cell count.
- Urine Test: A urinalysis can help rule out other conditions, such as a urinary tract infection.
- Imaging Tests: Imaging tests, such as a CT scan or ultrasound, can help visualize the appendix and surrounding tissues to confirm the diagnosis of appendicitis.
Treatment of Appendicitis:
The standard treatment for appendicitis is surgical removal of the appendix, known as an appendectomy.
- Open Appendectomy: Involves making a single incision in the lower right abdomen to remove the appendix.
- Laparoscopic Appendectomy: Involves making several small incisions in the abdomen and using a laparoscope (a thin, lighted tube with a camera) to guide the surgical instruments. Laparoscopic appendectomy is generally preferred because it results in less pain, a shorter hospital stay, and a faster recovery.
In some cases, if the appendicitis is mild and the patient is not severely ill, antibiotics may be used to treat the infection. However, surgery is usually necessary to prevent recurrence of the infection.
Complications of Appendicitis:
If left untreated, appendicitis can lead to serious complications, including:
- Rupture of the Appendix: The inflamed appendix can rupture, spilling infectious material into the abdominal cavity.
- Peritonitis: Inflammation of the lining of the abdominal cavity, caused by infection from a ruptured appendix. Peritonitis can be life-threatening.
- Abscess Formation: A collection of pus can form around the appendix, requiring drainage.
- Sepsis: A life-threatening response to infection that can lead to organ damage and death.
Prevention of Appendicitis:
There is no guaranteed way to prevent appendicitis, but some lifestyle factors may help reduce the risk:
- Eat a High-Fiber Diet: A diet rich in fruits, vegetables, and whole grains can promote healthy bowel function and reduce the risk of appendicitis.
- Stay Hydrated: Drinking plenty of water can help prevent constipation, which may contribute to appendicitis.
- Maintain a Healthy Weight: Obesity has been linked to an increased risk of appendicitis.
- Avoid Smoking: Smoking can increase inflammation in the body and may increase the risk of appendicitis.
The Role of Gut Health
The gut microbiome plays a critical role in overall health, including immune function and digestion. Maintaining a healthy gut microbiome may help reduce the risk of appendicitis.
- Probiotics: Probiotics are live microorganisms that can help restore the balance of the gut microbiome. They are found in fermented foods, such as yogurt, kefir, and sauerkraut, and are also available as supplements.
- Prebiotics: Prebiotics are non-digestible fibers that feed the beneficial bacteria in the gut. They are found in foods such as onions, garlic, asparagus, and bananas.
- Avoid Unnecessary Antibiotics: Antibiotics can kill both harmful and beneficial bacteria in the gut, disrupting the balance of the microbiome. It is important to use antibiotics only when necessary and as prescribed by a doctor.
Appendicitis in Children
Appendicitis is the most common cause of abdominal surgery in children. The symptoms of appendicitis in children are similar to those in adults, but children may have difficulty describing their symptoms.
In children, appendicitis can be more difficult to diagnose because they may not be able to pinpoint the location of the pain. They may also be more likely to have atypical symptoms, such as diarrhea or irritability.
If a child is suspected of having appendicitis, it is important to seek medical attention immediately.
Appendicitis in Pregnant Women
Appendicitis is a relatively rare but serious condition that can occur during pregnancy. The symptoms of appendicitis in pregnant women are similar to those in non-pregnant women, but the diagnosis can be more challenging because the symptoms can overlap with those of normal pregnancy.
Appendicitis during pregnancy can increase the risk of complications, such as preterm labor and delivery. Therefore, it is important to seek medical attention immediately if a pregnant woman is suspected of having appendicitis.
Conclusion
The increasing rates of appendicitis among Gen X and Millennials are a cause for concern. While the exact cause of this trend remains unclear, changes in diet, gut microbiome alterations, environmental factors, and an overactive immune system may all play a role.
Further research is needed to identify the specific factors driving this generational difference and to develop targeted prevention strategies. In the meantime, healthcare providers should be aware of the increased risk of appendicitis in younger adults and should ensure timely diagnosis and treatment. Promoting healthy lifestyle choices, such as a balanced diet and regular exercise, may also help reduce the risk of appendicitis.
Frequently Asked Questions (FAQ)
1. Why are Gen X and Millennials more likely to get appendicitis compared to their parents?
The exact reasons are still under investigation, but potential factors include changes in diet (more processed foods, less fiber), alterations in the gut microbiome, increased exposure to environmental toxins, a more reactive immune system due to less exposure to infections in childhood (the “hygiene hypothesis”), and delayed childbearing. The study suggests “generational risk factors at play that are contributing to this rise,” indicating a complex interplay of environmental and lifestyle influences specific to these generations.
2. What are the main symptoms of appendicitis that I should be aware of?
The most common symptoms include abdominal pain (typically starting near the belly button and moving to the lower right abdomen), nausea, vomiting, loss of appetite, fever, and abdominal tenderness. However, not everyone experiences all of these symptoms, and they can vary.
3. How is appendicitis diagnosed?
Diagnosis usually involves a physical examination by a doctor to check for tenderness, blood tests to look for signs of infection (like elevated white blood cell count), and imaging tests such as a CT scan or ultrasound to visualize the appendix. A urine test may also be performed to rule out other conditions.
4. What is the treatment for appendicitis, and are there alternatives to surgery?
The standard treatment is surgical removal of the appendix, called an appendectomy. This can be done through a traditional open incision or laparoscopically (using small incisions and a camera). In some mild cases, antibiotics may be used initially, but surgery is often necessary to prevent recurrence and potential complications.
5. Can I prevent appendicitis?
There’s no guaranteed way to prevent it, but adopting a healthy lifestyle might help. This includes eating a high-fiber diet rich in fruits, vegetables, and whole grains, staying hydrated, maintaining a healthy weight, and avoiding smoking. Supporting a healthy gut microbiome through probiotics and prebiotics may also be beneficial.